If you have golf swing-related Low Back Pain/Injury, this is a must-read article.
The following is an excerpt from my LPGA Master Thesis titled:
“The Mechanics of Golf Swing Related Injury: A Literature Review, Synthesis and Analysis”
(the entire paper at: https://jacc-ojs-twu.tdl.org/jacc/article/view/201901
I looked through 869 research papers for this LITERATURE REVIEW study that collated all the epidemiology, etiology and biomechanics of golf swing-related injury at all major joints.
Lumbar Spine Pain/Injury – An Introduction plus the Epidemiology
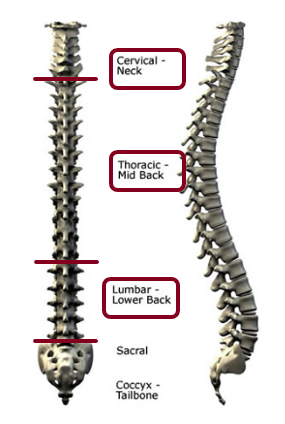
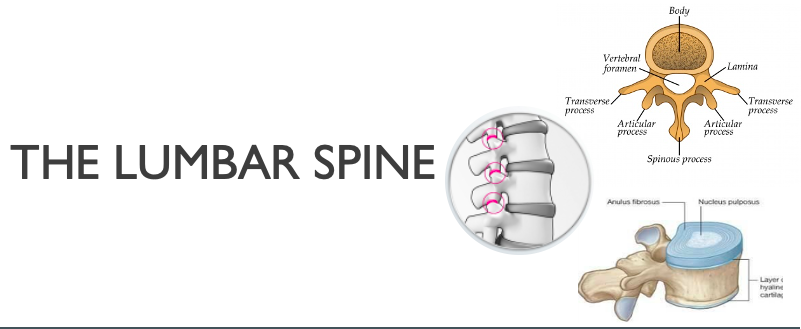
The spine, consisting of 33 segments termed “vertebrae”, is divided into five regions – cervical, thoracic, lumbar, sacral and coccygeal – based on the general design of the vertebrae in these regions. The vertebral bodies of the cervical (except the first two), thoracic and lumbar vertebrae are separated by intervertebral discs, and the bodies are also connected, on their posterior aspects, through articulations known as facet joints. Movement of the spine is facilitated by motion at the discs and facet joint structures, while the ligaments (fibrous tissue connecting two or more bones) act to restrain excessive movement (Armstrong, 1994). Armstrong stated that typically seen golf-related LBP was either spondylogenic or discogenic. He further described spondylogenic pain as either emanating from changes to vertebral bones or from degeneration to muscles, ligaments or fascia (fibrous tissue surrounding muscle). Discogenic pain results from intervertebral disc degeneration or herniation (protrusion).
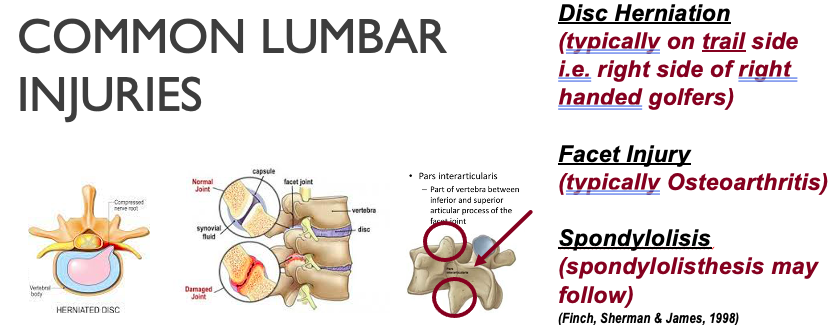
An epidemiological study conducted in Australia (Finch, Sherman & James, 1998) was based on data collected from sports medicine clinics and hospital emergency departments. The researchers found that the lower back was the most frequently seen area of injury (in 25% of all cases seen). The lower back/lumbar spine pathologies were categorized as being either intervertebral disc or facet joint injuries, and typically resulted from overuse.
One study of elite and professional male and female Japanese golfers found that 55% of their questionnaire respondents had low back injury (Sugaya et al., 1998), with 22% of total cases being from each of the PGA (male) and LPGA (female) Tours of Japan, and 10% being from the senior PGA Tour of Japan. Of those with LBP, 51% had right-side symptoms, 28% left-side and 21% had central symptoms (all right-handed golfers), and those having right-side symptoms showed an association of pain with the impact and follow-through swing phases. The researchers found that right-handed golfers with LBP showed significantly higher right-side vertebral osteophyte (bony outgrowth/protuberance) formation and right-side facet joint osteoarthritis (OA) than non-golfing controls with LBP.
In a review article (Reed & Wadsworth, 2010) back pain was said to be caused by mechanical pain, which includes muscle strain/spasm, discogenic pain (involving an intervertebral disc), spondylogenic (degeneration of spine) pain, or pain related to facet arthropathy (pathology of a joint). In older golfers, hip OA may be a factor in LBP. Herniation of a disc can also cause LPB, as can spondylolysis (degeneration of the pars interarticularis part of a vertebra; typically seen in younger golfers), and spondylolisthesis (forward slip of a vertebra on the one below it) subsequent to bilateral spondylolysis. Facet joint pain, according to the review, can be similar to spondylolisis, and can manifest either as pain in the joints in younger athletes or as OA in older golfers. Additionally, the article also stated that sacroiliac joint dysfunction can account for up to 40% of low back injuries and is especially common among younger, more athletic golfers. Another review article stated that when golfers are aged 50 and above, they can suffer from vertebral compression fractures (Cabri, Sousa, Kots & Barreiros, 2009). Finally, one 1993 case study article (Ekin & Sinaki 1993) reported that three postmenopausal women suffered multiple vertebral compression fractures in the thoracic and upper lumbar regions while playing golf. This latter phenomenon was ascribed to reduced bone mineral density, not to swing mechanics.
Another review article (Tucker, 2016) specified that the paraspinal muscles (adjacent to the spinal column) typically sustain tears and strains. Moreover, besides the facet joint and lumbar disc injuries seen, when there is injury to the posterior arch of a vertebra, spondylolysis may result. Typically, then, LBP can be said to include disc, facet joint, or spondylolysis-related injuries in the overuse category.
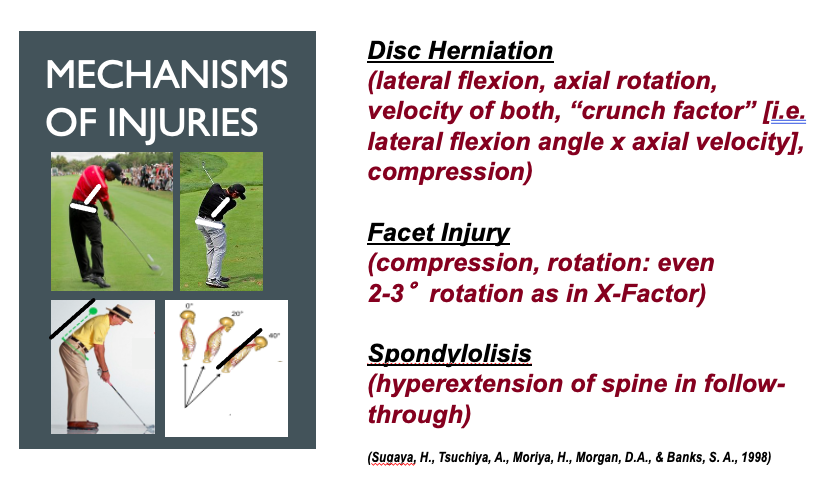
The Etiology
The lumbar spine, based on the design of its discs and facet joints, allows significant forward flexion and extension, some lateral flexion (side-bending) and limited horizontal plane axial rotation (Gluck, Bendo, & Spivak, 2008). In the context of those specific capabilities and limitations, the four directionally different forces imposed on the lumbar region of the spine during the golf swing are: shear forces directed anteroposteriorly (front-to-back), shear forces directed mediolaterally (side-to-side), vertical compressive forces (caused by back muscles that pull downwards to stabilize the body from falling forwards), and torsional forces around the vertical axis of the body (Hosea, Gatt & Gertner, 1994). As a point of distinction, “axial loading” involves compression along the vertical axis of the body, while “axial rotation” refers to rotation about the vertical axis (spinal column) of the body.
One early study (Sugaya et al., 1998) combined epidemiological findings with those of radiographs, to understand not only the prevalence of LBP, but also to discover the location of injury, the swing phase during which symptoms were reproduced, and the actual tissues injured during the golf swing. The authors concluded that the main contributing factor for lumbar degeneration and other injury was a combination of the lateral bending angle and rotational velocity of the torso, which they termed the “crunch factor”. The crunch factor increases during the downswing, and reaches peak values just after impact.
A subsequent study (Cole & Grimshaw, 2014) that further analyzed the crunch factor (related to lateral bending angle and trunk rotational velocity), compared golfers with and without LBP. Both groups showed increasing crunch factor from mid-downswing to impact and slightly beyond. The authors concluded, based on a comparison with a study of cricket fast bowlers, that lateral bending velocity combined with rotational velocity might be more predictive of injury and also opined that the iron clubs would cause more injury that the wood clubs because of the greater lateral bend and lateral bending velocity involved. Finally, a study comparing LBP in elite female cricket fast bowlers with and without LPB, concluded that it was lateral bending rather than shoulder counterrotation (angle between shoulders and pelvis, similar to that seen in golf’s X-Factor angle) which would be more likely to cause pain (Stuelcken, Ferdinands, & Sinclair, 2010). The X-Factor in golf involves a maximization of the hip-shoulder separation angle, tends to increase torque on the lumbar spine, and has been implicated in LBP in golfers (Gluck et al., 2008).

Lumbar disc trail side. Disc herniation has been ascribed to a combination of compression, torsion and lateral bending (Lee & Lee, 2017). As little information exists on the mechanisms of injury for the individual tissues injured, a report from other sports or from cadaveric studies is often useful. In a very early cadaveric study (Roaf, 1960), the author stated that the healthy disc, as well as vertebral joints and ligaments are resistant to compression and stretching created by spinal flexion and extension, but vulnerable to rotation and horizontal (side-to-side) shear. The lumbar disc, specifically, is fairly resistant to a compressive force, and prolapse (sinking down) takes place only if its inner nucleus pulposus has lost its typical turgor, such as occurs with aging. Conversely, according to the author, a combination of rotation and compression can cause most spinal injuries.
One review paper (Gluck et al., 2008) also stated that disc herniation in a healthy disc typically takes place as a result of lateral bending combined with compression and torsion, all of which, the authors remarked, may be seen during the golf swing. Finally, Lindsay and Vandervoort (2014), mentioned that compression loads (higher in professionals than in amateurs) may also cause disc herniation, because such loads, seen across all skill levels of golfers, are greater than those found in a cadaveric study to cause disc prolapse. The authors also suggested that the side bend seen in the golf swing causes mediolateral shear, which may be harmful to the discs, as it is mainly those structures, not vertebral bone, that resist sideward-directed forces. Thus downswing lateral flexion with axial rotation, the velocities of both movements, and compressive forces, are the main factors implicated in lumbar disc herniation.
Lumbar facet joint trail side. As the lumbar spine is not designed for rotation, (Gluck et al., 2008) specifically because of the sagittal (front-to-back) orientation of its facet joints, even a 2º to 3º intersegmental rotation (as seen in any swing using limited pelvis versus large torso
rotation, termed the X-Factor in golf) can produce facet joint microtrauma. Facet joint pain can be similar to pain from spondylolysis, according to one review article (Reed & Wadsworth, 2010), and is caused mainly by hyperextension, although compression and rotation can be precipitating factors too.
Lumbar spondylolysis. Based on his cadaveric study, Roaf, (1960), believed that the
so-called hyperextension (as seen in the “reverse-C” finish of the modern golf swing) and hyperflexion injuries are really rotation injuries. However, according to a prospective study of injury incidence among pole vaulters of both genders, a spodylolytic fracture results fromrepetitive hyperextension of the lumbar spine (Rebella, 2015). A golf review article (Reed & Wadsworth, 2010) summarized the information by stating that spondylolysis, which typically occurs in younger golfers, is caused by repeated lumbar hyperextension, and exacerbated with rotation.